WELCOME!
Our physicians are highly trained to provide leading-edge
care for all ages.

About
Lansing Foot & Ankle Center has been treating Chicagoland patients for their foot and ankle problems since 1985. Our experience and training have allowed our podiatric physicians & surgeons to provide complete medical and surgical care for all foot, ankle and lower leg conditions. We are the premiere podiatric group for treating any injuries involving bone, vascular, dermatological and soft tissue. With multiple podiatric physicians to treat you, we can offer scheduling flexibility and a doctor-patient match that suits your lifestyle. Many of our patients drive great distances to experience the highest level of treatment. Please consider that your feet are your primary mode of transportation and we urge you to take the time to evaluate Lansing Foot & Ankle Center. We are the choice of many happy patients and numerous satisfied doctors, many of whom have become our patients as well.
Our Services
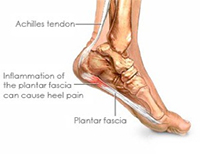 The most common cause of pain on the bottom surface of the heel, is plantar fasciitis (inflammation of the plantar fascia). The most common symptom of plantar fasciitis is heel pain experienced while standing/walking after sitting for a period of time or arising out of bed. The plantar fascia a broad band of ligament-like tissue which runs along the bottom surface of the foot, from the heel to the toes. Long standing inflammation may cause the formation of a heel spur which is visible on x-ray. Treatment may include custom made inserts (orthotics), oral anti-inflammatory medication, cortisone injections, or surgery. In most cases, non-surgical treatment is successful.
The most common cause of pain on the bottom surface of the heel, is plantar fasciitis (inflammation of the plantar fascia). The most common symptom of plantar fasciitis is heel pain experienced while standing/walking after sitting for a period of time or arising out of bed. The plantar fascia a broad band of ligament-like tissue which runs along the bottom surface of the foot, from the heel to the toes. Long standing inflammation may cause the formation of a heel spur which is visible on x-ray. Treatment may include custom made inserts (orthotics), oral anti-inflammatory medication, cortisone injections, or surgery. In most cases, non-surgical treatment is successful.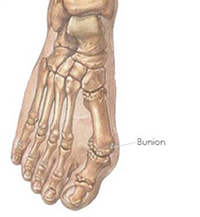 A bunion is a condition that affects the bones and joints associated with the great toe. It is one of the most common deformities of the foot. The condition develops slowly and results from the gradual dislocation of the big toe joint. The big toe drifts away from the body’s mid-line (and toward the smaller toes). This causes a prominence of bone on the inside (medial) margin of the forefoot. This is termed a bunion. As the deformity progresses, the big toe may push against the second toe or may overlap or under lap the second toe. There are no exercises, splints or other devices that reliably correct a bunion. Orthotics can sometimes slow or halt the progression of a bunion while pads, cortisone injections and changes in shoe widths may offer some relief. If a patient has a bunion that causes continued pain, Ridgeland Foot & Ankle doctors offer the newest corrective surgical techniques that allow most patients to walk during their entire recovery period. We have the experience to correct bunions or to repair bad results from a patient’s previous bunion surgery.
A bunion is a condition that affects the bones and joints associated with the great toe. It is one of the most common deformities of the foot. The condition develops slowly and results from the gradual dislocation of the big toe joint. The big toe drifts away from the body’s mid-line (and toward the smaller toes). This causes a prominence of bone on the inside (medial) margin of the forefoot. This is termed a bunion. As the deformity progresses, the big toe may push against the second toe or may overlap or under lap the second toe. There are no exercises, splints or other devices that reliably correct a bunion. Orthotics can sometimes slow or halt the progression of a bunion while pads, cortisone injections and changes in shoe widths may offer some relief. If a patient has a bunion that causes continued pain, Ridgeland Foot & Ankle doctors offer the newest corrective surgical techniques that allow most patients to walk during their entire recovery period. We have the experience to correct bunions or to repair bad results from a patient’s previous bunion surgery.
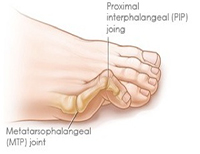 A hammertoe is a condition in which the toe buckles, causing the middle joint of the affected toe to poke up. Often a corn or callus develops on the top of the toe or the tip of the toe or under the ball of the foot behind a hammertoe. Pads, orthotics, corn/callus scraping, shoe modifications, cortisone injections or easy surgical procedures often provide periodic or permanent relief.
A hammertoe is a condition in which the toe buckles, causing the middle joint of the affected toe to poke up. Often a corn or callus develops on the top of the toe or the tip of the toe or under the ball of the foot behind a hammertoe. Pads, orthotics, corn/callus scraping, shoe modifications, cortisone injections or easy surgical procedures often provide periodic or permanent relief.
 This is a thickening of the surface layer of the skin, usually in response to pressure or friction. Corns or calluses may form on the ball of the foot, the heel, the top or tip of a toe. Calluses may be simple thickening of the skin. Sometimes they have a deep seated “core”. They can be the result of a wart or a boney prominence. They may also be formed by soft tissue masses that require a biopsy or removal. Many of the conditions mentioned in this website (bunions, hammertoes, warts, e.g.) may be the cause of the corn or callus. Scraping or shaving the callus offers periodic relief and simple procedures may offer permanent results. Diabetics should never attempt to scrape or cut their calluses/corns or use acid corn remover pads (most of these pads advise diabetic patients to not use their products). Diabetic patients should follow their primary care physician’s or family doctor’s recommendations and seek treatment from a qualified podiatrist.
This is a thickening of the surface layer of the skin, usually in response to pressure or friction. Corns or calluses may form on the ball of the foot, the heel, the top or tip of a toe. Calluses may be simple thickening of the skin. Sometimes they have a deep seated “core”. They can be the result of a wart or a boney prominence. They may also be formed by soft tissue masses that require a biopsy or removal. Many of the conditions mentioned in this website (bunions, hammertoes, warts, e.g.) may be the cause of the corn or callus. Scraping or shaving the callus offers periodic relief and simple procedures may offer permanent results. Diabetics should never attempt to scrape or cut their calluses/corns or use acid corn remover pads (most of these pads advise diabetic patients to not use their products). Diabetic patients should follow their primary care physician’s or family doctor’s recommendations and seek treatment from a qualified podiatrist.
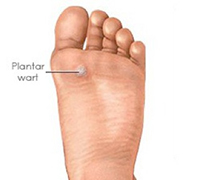 Warts are often found on the bottom of the foot, but can occur anywhere on the body. Warts are caused by a highly contagious virus (human papilloma virus or HPV). Treatment may include acid applications, freezing treatments, scraping or excision under local anesthetic, and laser surgery. Lumps and masses of the foot or around the ankle are often bursas, ganglion cysts, inclusion cysts, fibromas or lipomas. Ganglion cysts are best thought of as sacks of fluid from tendons or joints under the skin. While they are not generally harmful, they can be painful. Bursas are small sacks of fluid that the body produces to cushion prominent bones or protect tendons from irritation. On occasion they can become inflamed and irritated themselves. Inclusion cysts form when the body walls off a foreign body like a splinter, piece of glass or metal. Fibromas and lipomas are commonly occurring masses of fibrous or fatty tissue and frequently occur around the ankle or the bottom of the foot. There are many other kinds of masses. It is difficult to definitively diagnose a mass without microscopic examination. Often, experience, x-rays or MRI’s tell the doctor what type of mass the patient is presenting. Pads, cortisone injections or surgical removal of the mass may provide relief.
Warts are often found on the bottom of the foot, but can occur anywhere on the body. Warts are caused by a highly contagious virus (human papilloma virus or HPV). Treatment may include acid applications, freezing treatments, scraping or excision under local anesthetic, and laser surgery. Lumps and masses of the foot or around the ankle are often bursas, ganglion cysts, inclusion cysts, fibromas or lipomas. Ganglion cysts are best thought of as sacks of fluid from tendons or joints under the skin. While they are not generally harmful, they can be painful. Bursas are small sacks of fluid that the body produces to cushion prominent bones or protect tendons from irritation. On occasion they can become inflamed and irritated themselves. Inclusion cysts form when the body walls off a foreign body like a splinter, piece of glass or metal. Fibromas and lipomas are commonly occurring masses of fibrous or fatty tissue and frequently occur around the ankle or the bottom of the foot. There are many other kinds of masses. It is difficult to definitively diagnose a mass without microscopic examination. Often, experience, x-rays or MRI’s tell the doctor what type of mass the patient is presenting. Pads, cortisone injections or surgical removal of the mass may provide relief.
 Flatfoot is a common condition and is defined as an abnormal depression of the arch. These feet appear collapsed with excessive turning out of the heel, and the inside of the foot contacting the ground. It often has a genetic component. It may be initially asymptomatic, but often becomes progressively symptomatic with age. Some flat feet never become bothersome. The medial arch is unstable in flexible flatfoot, which creates stress on the surrounding soft-tissues and joints creating tired, sore arches. Flat feet may result in pain in the legs, knees, hips and lower back. Over the counter inserts may provide initial relief, but usually fail in providing long term results. Custom made orthotics (inserts) are usually the best method for treating this condition with surgery being reserved for severe cases.
Flatfoot is a common condition and is defined as an abnormal depression of the arch. These feet appear collapsed with excessive turning out of the heel, and the inside of the foot contacting the ground. It often has a genetic component. It may be initially asymptomatic, but often becomes progressively symptomatic with age. Some flat feet never become bothersome. The medial arch is unstable in flexible flatfoot, which creates stress on the surrounding soft-tissues and joints creating tired, sore arches. Flat feet may result in pain in the legs, knees, hips and lower back. Over the counter inserts may provide initial relief, but usually fail in providing long term results. Custom made orthotics (inserts) are usually the best method for treating this condition with surgery being reserved for severe cases.
 Skin infections have many causes. Because we rely on our feet for mobility, any skin disorder can cause severe limitations. Itching, sores, redness, swelling, fluid discharge and pain can rapidly present a serious medical condition. Fungal skin infections (athlete’s feet) are often confused with “dry skin” and may exist seasonally or for years. Most infections can be resolved with topical or oral medications, while serious infections may require tissue removal and wound treatment.
Skin infections have many causes. Because we rely on our feet for mobility, any skin disorder can cause severe limitations. Itching, sores, redness, swelling, fluid discharge and pain can rapidly present a serious medical condition. Fungal skin infections (athlete’s feet) are often confused with “dry skin” and may exist seasonally or for years. Most infections can be resolved with topical or oral medications, while serious infections may require tissue removal and wound treatment.

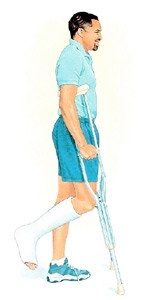
With 38 bones in a single foot, almost any of them can be broken. Many fractures do not require surgery, or even a cast, as they will heal on their own with some support. When a foot is fractured, the site of the fracture usually is painful and swollen. On occasion, a patient may not experience significant pain with a fracture. It is a common mistaken belief that one cannot walk with a fracture. The site and severity of the fracture (determined by in-office x-rays or referral to a MRI facility) will determine the course of treatment which may include taping, a cast shoe, a cast boot, or surgery.
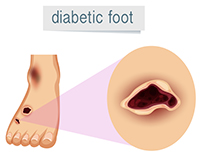
Diabetics can enjoy a lifetime of good health if they educate themselves and adopt proper regimens. Those with diabetes, especially those with poor control of their disease, have a high risk of eye disease, kidney disease and amputation. It is estimated that 15% of diabetics will undergo an amputation of the foot or leg and the diabetic population is ever increasing in the United States. Diabetics are recommended to visit a podiatrist routinely for nail and skin care. Even the smallest of cuts, ingrown nails, skin rashes or structural changes may result in a rapidly progressing problem. Non-healing skin ulcers, infections, redness, swelling, numbness, tingling and pain may be some of the problems a diabetic experiences. Often, a diabetic does not experience pain when encountering a severe problem (infections, skin wounds, e.g.) because of commonly occurring diabetic foot numbness (diabetic neuropathy). A foot doctor is often the first physician to recognize a problem before it becomes severe. Simple visits can prevent major problems.
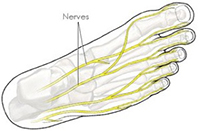
Numbness is often experienced by diabetics, but other patient types may experience the condition. Numbness and tingling can be the source of bothersome irritation, but more importantly, it reduces our ability to detect pain. Without pain, diabetics (or any patients suffering from neuropathy) could encounter cuts, sores, fractures, foreign bodies (splinters, tacks, needles, glass), calluses, infections, ingrown nails or other problems without knowledge. Anyone with numbness is urged to check their shoes daily and examine their feet (particularly the bottoms) and visit a podiatrist. Treatment may include oral medication, routine care, orthotics, and shoe changes. Numbness or tingling may also be caused by an isolated impinged nerve, a neuroma (or nerve growth), swelling, medication/alcohol side effects, injury or other conditions.

Thickened, brittle, flaking and discolored nails are often the cause of fungus. Most often, antifungal topical creams and polishes fail at reducing or resolving the fungus. If a fungus greatly thickens the nail, a patient cannot cut their nails properly and experiences pain and infections. A podiatrist can successfully cut significantly thickened nails and provide current and safe treatment options including prescription polishes, oral medication and routine care.
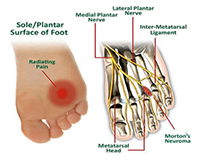
Morton’s Neuroma is a pathological condition of the common foot nerve between the third and fourth metatarsals/toes. The nerve sheath becomes abnormally thickened with fibrous (“scar”) tissue and the nerve fibers eventually deteriorate. This common foot nerve runs along the bottom surface of the foot and branches to supply sensation to the tips of the third and fourth toes. Occasionally, other foot nerves become affected. The patient complains of shooting pains or numbness at the ball of the foot (particularly at the area behind the third and fourth toes). Treatment often includes orthotics, cortisone injections, oral anti-inflammatory medications, and/or padding. Most often surgery can be avoided, but is considered in severe cases.

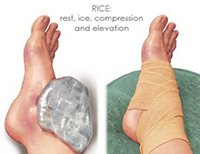
Many injuries and medical problems may cause ankle pain. Among them include Achilles tendonitis and ankle joint arthritis. Fractures, sports injuries, ankle sprains, tendonitis and ruptured ligaments may also reduce a patient’s ability to bear weight or walk. Immediate diagnosis is crucial to avoid persistent pain for months or years. In-office x-rays or MRI’s often provide answers and treatment may include immobilization (taping, casting, ankle braces), physical therapy, oral medications, cortisone injections, arthroscopic surgery or other surgical procedures.
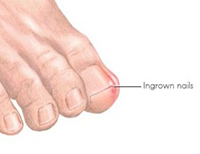
Ingrown toenails are caused by impingement of the skin along the margins of the nail by the nail plate. Some ingrown toenails are chronic, with repeated episodes of pain, inflammation, and infection. Infection results when inflamed tissues are colonized by bacteria or yeast. Pain can be present without infection, and occasionally infection is present without pain. An ingrown nail may seem trivial, but in the presence of other illnesses (diabetes or vascular/circulation problems), the condition may result in serious infection or amputation. Treatment is very simple and usually involves removal of a portion of the nail under local anesthetic. If the infection is severe or the patient is immunocompromised, oral antibiotics may be prescribed.
Immediate diagnosis and thorough documentation is necessary to protect a patient’s interests if an injury should occur at work. In-office x-rays and other tests may be important in ensuring that a patient has proof that an injury is legitimate and that they achieve proper healing.
- Cortisone injections
- X-rays (in-office)
- Custom made inserts (orthotics)
- Physical therapy referrals
- MRI/CT scan/bone scan referrals
- Second opinions
- Leg casts
- In office surgical procedures
- – Hospital procedures
- – On call Dr. 24/7
Meet Our Experts
Dr. Hye Jin Yoo
Dr. Hye Jin Yoo
Practice: Medical & surgical treatment of the foot & ankle
Experience: 4 years of experience
States Licensed: Illinois
Languages: English & Korean
Schooling: Undergrad- Villanova University / Med School – New York College of Podiatric Medicine
Residency: Ascension Providence Hospital in Southfield & Novi, Michigan

Dr. Harpreet Khalsa
Dr. Harpreet Khalsa
Practice: Medical & surgical treatment of the foot & ankle
Experience: 7 years of experience
States Licensed: Illinois and Indiana
Languages: English, Hindi & Punjabi
Schooling: Undergrad – Indiana University / Med School – Kent State University College of Podiatric Medicine
Residency: United Health Service Hospital surgical residency, New York
Dr. Mark Camilleri
Dr. Mark Camilleri
Practice: Medical & surgical treatment of the foot & ankle
Experience: 28 years of experience
States Licensed: Illinois
Languages: English & Spanish
Schooling: Undergrad – Michigan State University / Med School – Rosalind Franklin University
Residency: Edgewater Medical Center surgical residency, Illinois
OFFICE HOURS:
Mon – Sat: Daytime and Evening hours available
Sun: Closed
SCHEDULE AN APPOINTMENT
Call 708-474-1040 now to schedule an appointment.
24X7 EMERGENCY
We provide a 24 hour answering service with an on-call podiatric physician 24 hours a day/365 days a year.
INSURANCE & PAYMENT
We accept most insurance plans, major credit cards and cash.